Approximately 90% of people in the United States consume too much salt, which is the main source of sodium for the body.
While the effects may not be immediately noticeable, long-term excessive salt intake can lead to health problems, such as hypertension (high blood pressure), which affects half of the adult population in the U.S.
Certain symptoms may indicate high sodium levels, including persistent thirst, fatigue, headaches, heart palpitations, and swelling.
Reducing your salt intake—particularly from processed foods high in sodium—can help manage blood pressure and lower the risk of heart disease and other related health issues.
Thirst and Dehydration
Sodium plays a key role in regulating fluid balance within and outside of cells.
Excessive salt intake without sufficient fluid intake can lead to dehydration, as it draws water from cells.
Signs of dehydration include increased thirst, dry mouth, dry skin, and sunken eyes.
Headaches
High sodium levels can contribute to headaches, often due to dehydration.
These headaches are usually dull and constricting, accompanied by dizziness, irritability, and brain fog.
In severe cases of high blood pressure, a hypertensive crisis can trigger a sudden, intense headache, along with vomiting, chest pain, and seizures.
Cutting back on sodium may also help reduce chronic headaches in people with hypertension.
Fatigue
When sodium levels are too high, fatigue and weakness are common, especially in cases of hypernatremia (elevated sodium levels in the blood).
This condition can lead to brain swelling, also known as cerebral edema, causing fatigue and muscle weakness.
While dehydration is often the cause of hypernatremia, it’s typically not caused by sodium intake alone.
Heart Palpitations
As an electrolyte, sodium is essential for muscle contractions and heartbeats.
Excessive sodium can disrupt the balance between sodium and calcium in the blood, leading to irregular heartbeats, or palpitations.
Though these palpitations are often harmless, frequent or severe instances may result in dizziness, chest pain, cold sweats, or even fainting.
Bloating and Swelling
A high-sodium diet can lead to fluid retention, causing bloating and swelling.
This may result in puffiness, particularly around the eyes.
In individuals with severe heart, liver, or kidney conditions, fluid retention can cause peripheral edema (fluid buildup in the legs, ankles, and feet).
Excessive sodium can also cause gastrointestinal bloating and gas.
Weight Gain
Fluid retention caused by excessive salt intake may lead to temporary weight gain.
A study showed that increasing sodium intake by just 1 gram per day raised the risk of obesity.
The exact connection between increased sodium and fat accumulation requires more research.
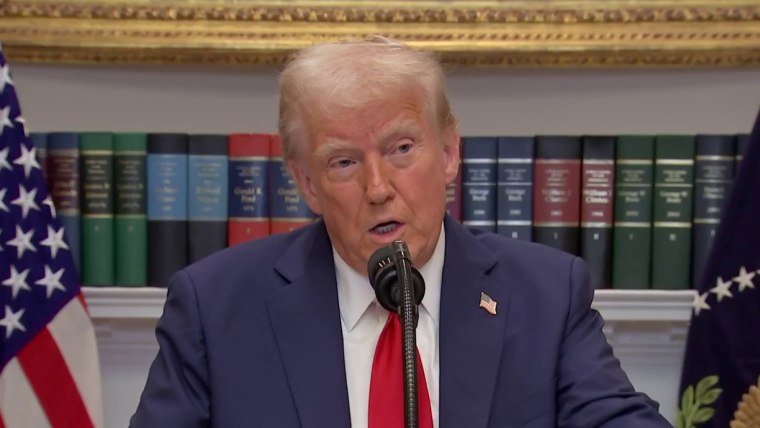
High Blood Pressure
High sodium intake causes the body to retain more fluid, which increases blood volume and raises blood pressure, potentially resulting in hypertension.
The World Health Organization associates sodium consumption above 5 grams per day with an increased risk of hypertension and cardiovascular issues.
Reducing sodium intake can significantly lower blood pressure and reduce the risk of heart disease within weeks.
Digestive Problems
In addition to bloating and weight gain, high sodium levels can cause nausea, upset stomach, and diarrhea due to fluid overload in the digestive system.
Excess sodium can also disrupt the gut microbiome, impairing nutrient absorption and leading to bloating, cramping, and gas.
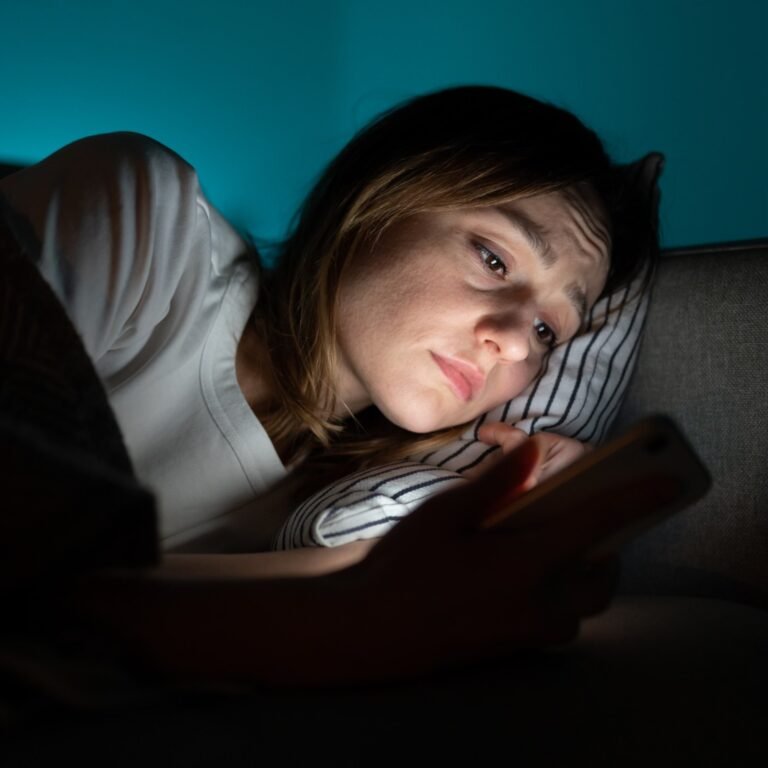
Sleep Disturbances
Excess sodium can disrupt sleep by contributing to fluid retention and high blood pressure.
As you lie down, fluid from the legs may move to the upper airways, increasing the risk of obstructive sleep apnea.
High blood pressure may also cause chest pain and headaches, further interfering with sleep.
Some studies suggest that too much sodium can disrupt the production of norepinephrine, a hormone that helps regulate sleep-wake cycles, leading to fragmented sleep.